


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 14-11-2021
Date: 5-11-2021
Date: 7-11-2021
|
Hypoglycemia Types
Hypoglycemia may be divided into four types: 1) insulin induced, 2) postprandial (sometimes called reactive hypoglycemia), 3) fasting hypoglycemia, and 4) alcohol related.
1. Insulin-induced hypoglycemia: Hypoglycemia occurs frequently in patients with diabetes who are receiving insulin treatment, particularly those striving to achieve tight control of blood glucose levels. Mild hypoglycemia in fully conscious patients is treated by oral administration of carbohydrate. Unconscious patients are typically given glucagon subcutaneously or intramuscularly (Fig. 1).
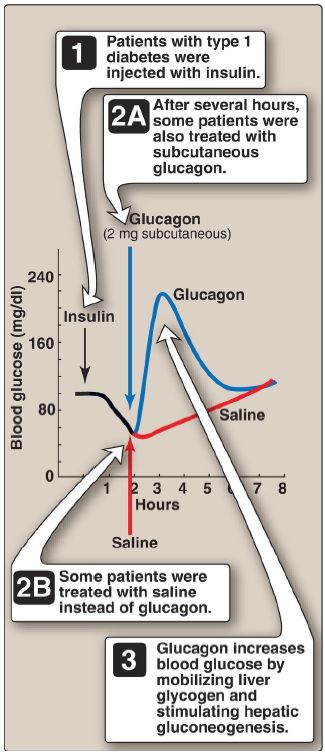
Figure 1: Reversal of insulin-induced hypoglycemia by administration of subcutaneous glucagon.
2. Postprandial hypoglycemia: This is the second most common form of hypoglycemia. It is caused by an exaggerated insulin release following a meal, prompting transient hypoglycemia with mild adrenergic symptoms. The plasma glucose level returns to normal even if the patient is not fed. The only treatment usually required is that the patient eats frequent small meals rather than the usual three large meals.
3. Fasting hypoglycemia: Low blood glucose during fasting is rare but is more likely to present as a serious medical problem. Fasting hypoglycemia, which tends to produce neuroglycopenic symptoms, may result from a reduction in the rate of glucose production by hepatic glycogenolysis or gluconeogenesis. Thus, low blood glucose levels are often seen in patients with hepatocellular damage or adrenal insufficiency or in fasting individuals who have consumed large quantities of ethanol (see 4. below). Alternately, fasting hypoglycemia may be the result of an increased rate of glucose use by the peripheral tissues because of overproduction of insulin by rare pancreatic tumors. If left untreated, a patient with fasting hypoglycemia may lose consciousness and experience convulsions and coma. [Note: Certain inborn errors of metabolism, for example, defects in FA oxidation, result in fasting hypoglycemia.]
4. Alcohol-related hypoglycemia: Alcohol (ethanol) is metabolized in the liver by two oxidation reactions (Fig. 2). Ethanol is first converted to acetaldehyde by zinc-containing alcohol dehydrogenase. Acetaldehyde is subsequently oxidized to acetate by aldehyde dehydrogenase (ALDH).
[Note: ALDH is inhibited by disulfiram, a drug that is used in the treatment of chronic alcoholism. The resulting rise in acetaldehyde results in flushing, tachycardia, hyperventilation, and nausea.] In each reaction, electrons are transferred to oxidized nicotinamide adenine dinucleotide (NAD+), resulting in an increase in the ratio of the reduced form (NADH) to NAD+. The abundance of NADH favors the reduction of pyruvate to lactate and of oxaloacetate (OAA) to malate. Recall from that pyruvate and OAA are substrates in the synthesis of glucose. Thus, the ethanol-mediated increase in NADH causes these gluconeogenic precursors to be diverted into alternate pathways, resulting in the decreased synthesis of glucose. This can precipitate hypoglycemia, particularly in individuals who have depleted their stores of liver glycogen. [Note: Decreased availability of OAA allows acetyl CoA to be diverted to ketone body synthesis in the liver and can result in alcoholic ketosis that may result in ketoacidosis.]
Hypoglycemia can produce many of the behaviors associated with alcohol intoxication, such as agitation, impaired judgment, and combativeness. Therefore, alcohol consumption in vulnerable individuals (such as those who are fasted or have engaged in prolonged, strenuous exercise) can produce hypoglycemia that may contribute to the behavioral effects of alcohol. Because alcohol consumption can alsoincrease the risk for hypoglycemia in patients using insulin, those in an intensive insulin treatment protocol are counseled about the increased risk of hypoglycemia that generally occurs many hours after alcohol ingestion.
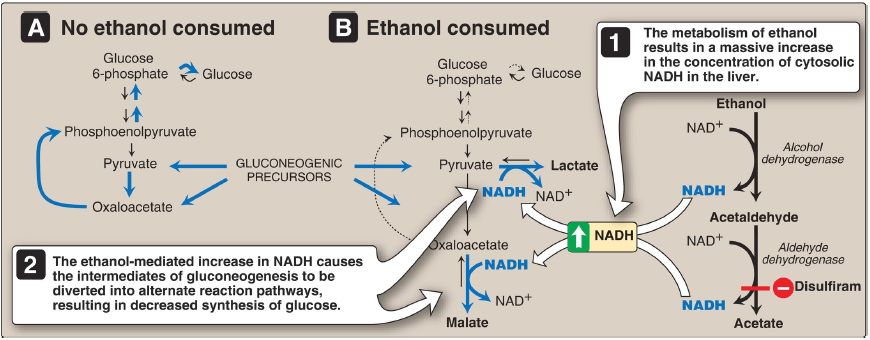
Figure 2: A. Normal gluconeogenesis in the absence of ethanol consumption. B. Inhibition of gluconeogenesis resulting from hepatic metabolism of ethanol. NAD(H) = nicotinamide adenine dinucleotide.
Chronic alcohol consumption can also result in alcoholic fatty liver because of increased hepatic synthesis of TAG coupled with impaired formation or release of VLDL. This occurs as a result of decreased FA oxidation because of a fall in the NAD+/NADH ratio and increased lipogenesis because of the increased availability of FA (decreased catabolism) and of glyceraldehyde 3-phosphate (the dehydrogenase is inhibited by the low NAD+/NADH ratio). With continued alcohol consumption, alcoholic fatty liver can progress first to alcoholic hepatitis and then to alcoholic cirrhosis.



|
|
|
|
للعاملين في الليل.. حيلة صحية تجنبكم خطر هذا النوع من العمل
|
|
|
|
|
|
|
"ناسا" تحتفي برائد الفضاء السوفياتي يوري غاغارين
|
|
|
|
|
|
|
نحو شراكة وطنية متكاملة.. الأمين العام للعتبة الحسينية يبحث مع وكيل وزارة الخارجية آفاق التعاون المؤسسي
|
|
|